Mergers can affect funding, staffing and patient populations at state’s federally qualified community health centers
By Kelly Burch-Granite State News Collaborative
Since Catholic Medical Center in Manchester was purchased by the national for-profit HCA Healthcare in February, Manchester’s low-income patients have faced some uncertainty.
In the past, patients seen at Amoskeag Health, Manchester’s community health center, could get approved for reduced copays based on their income. Catholic Medical Center would honor those reduced copays, removing a hassle and streamlining patients’ access to affordable care at the hospital, said Kris McCracken, president and CEO at Amoskeag Health.
Since the merger, the use of that program has been paused.
“I hope we can establish a similar arrangement with HCA … [but] I haven’t even met with them yet,” said McCracken. “You’ve got to rebuild that relationship.”
That’s just one example of the way that hospital mergers around the state are affecting New Hampshire’s 11 federally qualified community health centers. They are seen as the safety net of the health care system, providing primary care to everyone, regardless of their ability to pay. The centers are funded primarily by federal grants and Medicaid reimbursements, but also rely on community benefit grants from local hospitals — some of which disappear after a merger occurs, FQHC leaders say.
In addition to affecting the grants, hospital mergers can lead to higher employment costs for the health centers, create a higher proportion of patients who are unable to pay (since for-profit organizations can decline to provide care for those people) and erode a sense of community cooperation between hospitals and the centers.
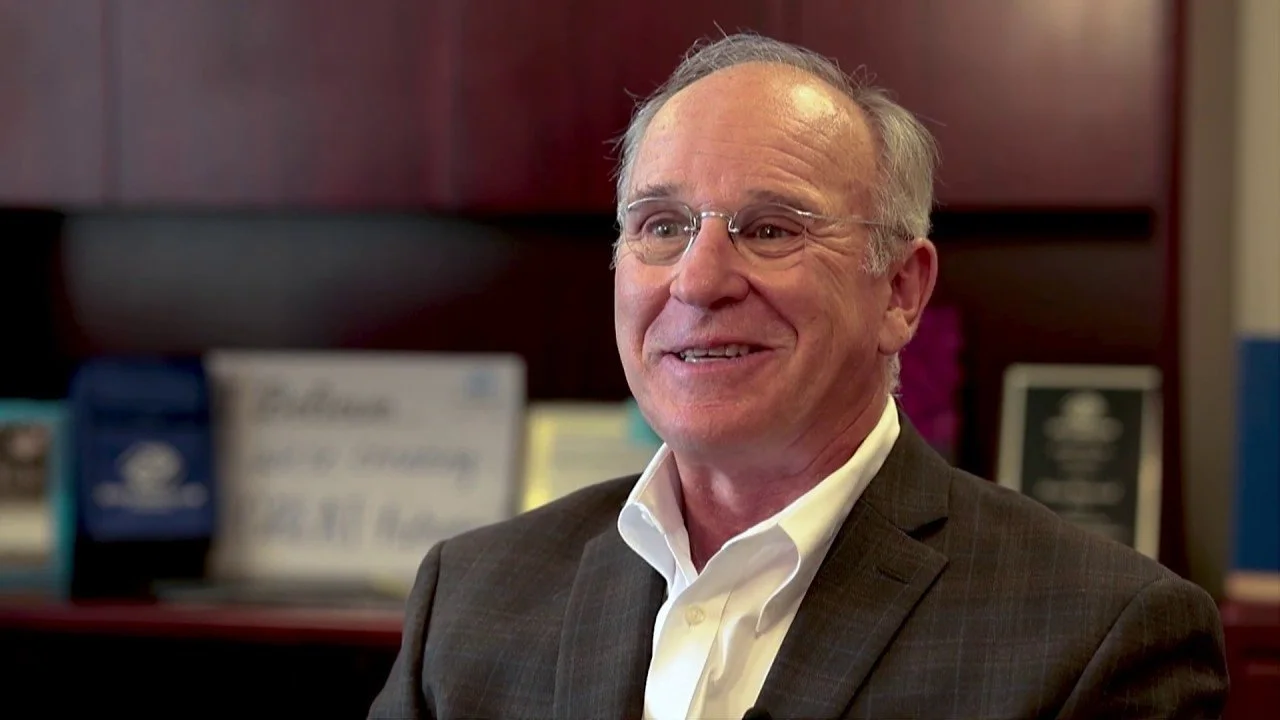
“As some of these mergers occur, it feels like the senior leadership gets a little further away from the community,” said Gregory White, CEO of Lamprey Health Center, a federally qualified health center with locations in Nashua, Newmarket and Raymond. “Sometimes when that happens, instead of doing things with you, [things] happen to you.”
While the challenges are real, leaders of the health centers also emphasize that, with work, there can be functional and cooperative relationships with larger hospital systems.
“Just because they’re a big health care system doesn’t mean they’re not a good partner,” McCracken said.
Loss of local control and local grants
One of the touchiest subjects when it comes to hospital mergers and federally qualified health centers involves community benefit grants. These grants are provided by hospitals to serve a specific community need. They also are a way of acknowledging the role that the community health centers play in the health care system, McCracken said.
If a community has two or three private practices, often linked to larger health care systems, the local community health center is “kind of taking the leftovers,” she said — patients who are uninsured or unable to pay for care. For the community health centers, there’s often no balance between paying patients and charitable care, she said.
“You’re the safety net for the folks who are the neediest in the community,” she said.
While that’s the role of the health centers, McCracken said, it requires support from the hospital systems that are benefiting from serving more profitable patients.
“We’re here to be the safety net … but if all we have is safety net patients, that means we need more community investment,” she said.
Amoskeag Health never received a community benefit grant from Catholic Medical Center, due to the hospital’s religious guidelines, and doesn’t anticipate receiving one from HCA, McCracken said. Amoskeag Health does receive grants from Dartmouth Health and Elliot Health System, which also gives a grant to Lamprey Health.
In the past, however, when hospitals have gone through mergers, “it felt like we lost touch with them,” and community benefit grants have gone away, White said. He, like many community health center leaders who spoke to the Granite State News Collaborative, declined to elaborate; some of them expressed concern about jeopardizing their relationship with hospitals, and thus access to future grants.
Changing patient populations and cost concerns
Ed Shanshala, CEO of Ammonoosuc Community Health Services Inc., has concerns about larger hospital organizations, especially for-profit companies, buying into the New Hampshire health care system. The ethical obligations to patients and legal obligations to shareholders are too difficult to balance, he said.
Ammonoosuc Community Health Services Inc. has locations in Littleton, Warren, Whitefield and Woodsville. The organization recently announced its Franconia location will close soon because of funding concerns.
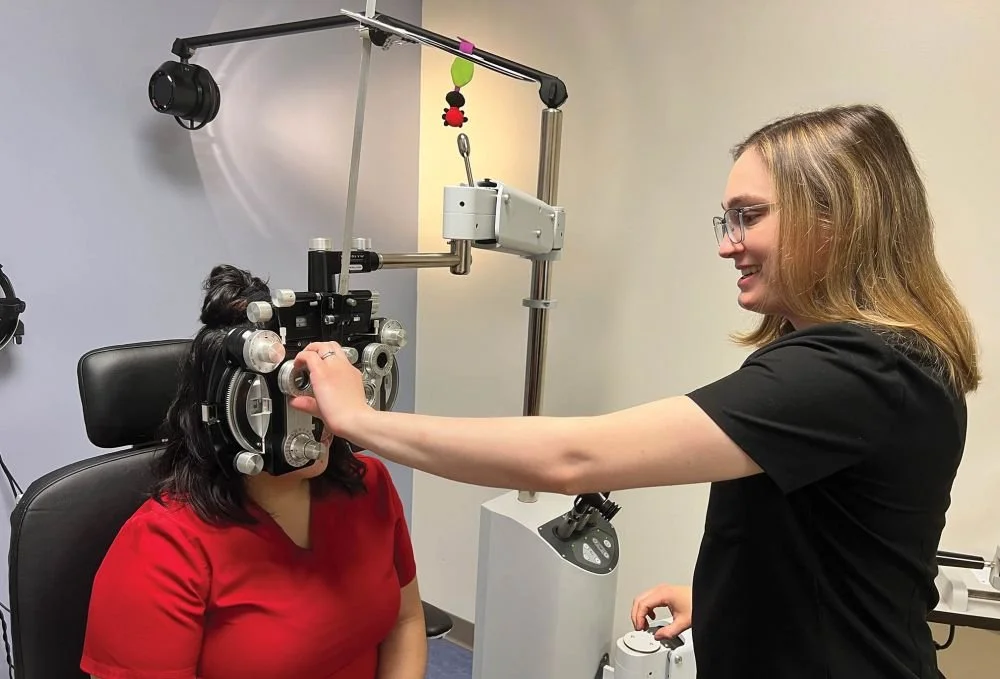
Jillian Peabody of Amoskeag Health with a patient. Low-income patients at the federally qualified health center in Manchester have faced uncertainty about their health care since the for-profit HCA Healthcare’s acquisition of Catholic Medical Center. (Courtesy of Amoskeag Health)
If for-profit hospitals are "going to carve out the most beneficial and profitable [patients], those of us who serve the collective are going to be left unable to serve the most vulnerable population,” Shanshala said.
Mergers can also affect where patients choose to receive care, and the services they have access to, said Robert MacLeod, CEO of Mid-State Health Center in Plymouth.
“We sometimes see increased costs and fewer choices, especially when systems prioritize keeping patients within their own network,” he said. “That can limit our ability to refer to the most appropriate or affordable specialty care, and in some cases, services like maternity care or certain specialties may be reduced based on financial pressures.”
MacLeod has another concern: that the buying power of large hospital systems could ultimately exclude federally qualified health centers from working with certain insurers.
“As larger systems gain more negotiating power with payers,” he said, federally qualified health centers “may find it harder to compete or collaborate under the same terms. We may face tighter reimbursement rates or be excluded from certain payer networks, even when we offer high-quality, cost-effective care.”
Shanshala is likewise skeptical of the widespread claims from hospital systems that mergers reduce costs.
“Although there’s been a promise of efficiencies through aggregation of health care, it’s not clear they’ve ever delivered on economies of scale, delivering on a lower price point for patients,” he said. “I’ve personally never experienced lower prices.”
Personnel costs are a massive burden for federally qualified health centers, taking up about three-quarters of operating budgets. Large health systems can make things even worse.
“With consolidation, especially very large players like Mass General, there’s pressure on salaries that we just can’t compete with,” said White. (Boston-based Massachusetts General Hospital acquired Dover’s Wentworth-Douglass Hospital in 2017.)
McCracken used an analogy: If federally qualified health centers are kayaks on a bay, large health care systems are like giant ocean liners, throwing such a wake that the kayaks are often rocked.
“It’s not that they’re trying to do anything to any of us,” she said, “but their presence is so overwhelming in the health care space.”
These articles are being shared by partners in the Granite State News Collaborative. For more information, visit collaborativenh.org.